Posted by Admin
in Sunday, December 13, 2009

TEMPERATURE
Body temperature represents the balance between heat produced by metabolism, muscular activity, and other factors and heat lost through the skin, lungs, and body wastes. A stable temperature pattern promotes proper function of cells, tissues, and organs; a change in this pattern usually signals the onset of illness.
Temperature can be measured with a mercury, an electronic digital, or a chemical-dot thermometer. Oral temperature in adults normally ranges from 97° to 99.5° F (36.1° to 37.5° C); rectal temperature, the most accurate reading, is usually 1° F (0.6° C) higher; axillary temperature, the least accurate, reads 1° to 2° F (0.6° to 1.1° C) lower; and tympanic temperature reads 0.5° to 1° (0.3° to 0.6° C) higher.
Temperature normally fluctuates with rest and activity. Lowest readings typically occur between 4 and 5 a.m.; the highest readings occur between 4 and 8 p.m. Other factors
also influence temperature, including gender, age, emotional conditions, and environment. Keep the following principles in mind. Women normally have higher temperatures than men, especially during ovulation. Normal temperature is highest in neonates and lowest in elderly persons. Heightened emotions raise temperature; depressed emotions lower it. A hot external environment can raise temperature; a cold environment lowers it.
Equipment
Thermometer (mercury, electronic, chemical-dot, or tympanic) • water-soluble lubricant or petroleum jelly (for rectal temperature) • facial tissue • disposable thermometer sheath or probe cover (except for chemical thermometer) • alcohol pad.
Preparation of equipment
If a thermometer is included in the admission pack, keep it at the patient's bedside and, on discharge, allow him to take it home. Otherwise, obtain a thermometer from the nurses' station or central supply department. If you use an electronic thermometer, make sure it's been recharged. (See Types of thermometers.)
Implementation
-
Explain the procedure to the patient, and wash your hands. If the patient has had hot or cold liquids, chewed gum, or smoked, wait 15 minutes before taking an oral temperature.
Using a mercury thermometer
-
Hold the thermometer between your thumb and index finger at the end opposite the bulb.
-
If the thermometer has been soaking in a disinfectant, rinse it in cold water. Rinsing removes chemicals that may irritate oral or rectal mucous membranes or axillary skin. Avoid using hot water because it expands the mercury, which could break the thermometer. Using a twisting motion, wipe the thermometer from the bulb upward.
-
Then quickly snap your wrist several times while holding the thermometer to shake it down to below 98° F (36.7° C). Shaking causes the mercury to descend into the bulb. The mercury will then expand in response to the patient's body temperature and be forced upward.
-
To use a disposable sheath, disinfect the thermometer with an alcohol pad. Insert it into the disposable sheath opening; then twist to tear the seal at the dotted line. Pull it apart.
Using an electronic thermometer
Using a chemical-dot thermometer
-
Remove the thermometer from its protective dispenser case by grasping the handle end with your thumb and forefinger, moving the handle up and down to break the seal, and pulling the handle straight out. Keep the thermometer sealed until use.
Using a tympanic thermometer
-
Make sure the lens under the probe is clean and shiny. Attach a disposable probe cover.
-
Stabilize the patient's head; then gently pull the ear straight back (for children up to age 1) or up and back (for children age 1 and older to adults).
-
Insert the thermometer until the entire ear canal is sealed. The thermometer should be inserted toward the tympanic membrane in the same way that an otoscope is inserted. Then press the activation button and hold it for 1 second. The temperature will appear on the display.
-
PEDIATRIC ALERT For infants younger than age 3 months, take three readings and use the highest.
Taking an oral temperature
-
Position the tip of the thermometer under the patient's tongue, as far back as possible on either side of the frenulum linguae. Placing the tip in this area promotes contact with superficial blood vessels and contributes to an accurate reading.
-
Instruct the patient to close his lips but to avoid biting down with his teeth. Biting can break the thermometer, cutting the mouth or lips or causing ingestion of broken glass or mercury.
-
Leave a mercury thermometer in place for at least 2 minutes or a chemical-dot thermometer in place for 45 seconds to register temperature; for an electronic thermometer, wait until the maximum temperature is displayed.
-
For a mercury thermometer, remove and discard the disposable sheath; then read the temperature at eye level, noting it before shaking down the thermometer. For an electronic thermometer, note the temperature; then remove and discard the probe cover. For the chemical-dot thermometer, read the temperature as the last dye dot that has changed color, or fired; then discard the thermometer and its dispenser case.
Taking a rectal temperature
-
Position the patient on his side with his top leg flexed, and drape him to provide privacy. Then fold back the bed linens to expose the anus.
-
Squeeze the lubricant onto a facial tissue to prevent contamination of the lubricant supply.
-
Lubricate about ½″ (1.3 cm) of the thermometer tip for an infant, 1″ (2.5 cm) for a child, or about 1½″ (3.8 cm) for an adult. Lubrication reduces friction and thus eases insertion. This step may be unnecessary when using disposable rectal sheaths because they're prelubricated.
-
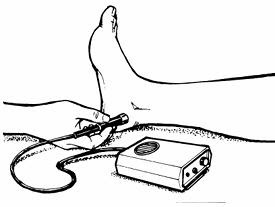
Lift the patient's upper buttock, and insert the thermometer about ½″ (1.3 cm) for an infant or 1½″ (3.8 cm) for an adult. Gently direct the thermometer along the rectal wall toward the umbilicus. This will avoid perforating the anus or rectum or breaking the thermometer. It will also help ensure an accurate reading because the thermometer will register hemorrhoidal artery temperature instead of fecal temperature.
-
Hold the mercury thermometer in place for 2 to 3 minutes, or the electronic thermometer until the maximum temperature is displayed. Holding the thermometer prevents damage to rectal tissues caused by displacement or loss of the thermometer into the rectum.
-
Carefully remove the thermometer, wiping it as necessary. Then wipe the patient's anal area to remove any lubricant or feces.
Taking an axillary temperature
-
Position the patient with the axilla exposed.
-
Gently pat the axilla dry with a facial tissue because moisture conducts heat. Avoid harsh rubbing, which generates heat.
-
Ask the patient to reach across his chest and grasp his opposite shoulder, lifting his elbow.
-
Position the thermometer in the center of the axilla, with the tip pointing toward the patient's head.
-
Tell him to keep grasping his shoulder and to lower his elbow and hold it against his chest. This promotes skin contact with the thermometer.
-
Remove a mercury thermometer after 10 minutes; remove an electronic thermometer when it displays the maximum temperature. Axillary temperature takes longer to register than oral or rectal temperature because the thermometer isn't enclosed in a body cavity.
-
Grasp the end of the thermometer and remove it from the axilla.