| CONDITION OR TREATMENT | PRECAUTIONARY PERIOD |
| Acquired immunodeficiency syndrome | Until white blood cell count reaches 1,000/ml or more, or according to facility guidelines |
| Agranulocytosis | Until remission |
| Burns, extensive noninfected | Until skin surface heals substantially |
| Dermatitis, noninfected vesicular, bullous, or eczematous disease (when severe and extensive) | Until skin surface heals substantially |
| Immunosuppressive therapy | Until patient's immunity is adequate |
| Lymphomas and leukemia, especially late stages of Hodgkin's disease or acute leukemia | Until clinical improvement is substantial |
CONDITIONS AND TREATMENTS REQUIRING NEUTROPENIC PRECAUTIONS
under:
Infection Control
NEUTROPENIC PRECAUTIONS
Posted by Admin
Unlike other types of precaution procedures, neutropenic precautions (also known as protective precautions and reverse isolation) guard the patient who is at increased risk for infection against contact with potential pathogens. These precautions are used primarily for patients with extensive noninfected burns, those who have leukopenia or a depressed immune system, and those receiving immunosuppressive treatments. (See Conditions and treatments requiring neutropenic precautions, page 130.)
Neutropenic precautions require a single room equipped with positive air pressure, if possible, to force suspended particles down and out of the room. The degree of precautions may range from using a single room, thorough hand-hygiene technique, and limitation of traffic into the room to more extensive precautions requiring the use of gowns, gloves, and masks by facility staff and visitors. The extent of neutropenic precautions may vary from facility to facility, depending on the reason for and the degree of the patient's immunosuppression.
To care for patients who have temporarily increased susceptibility, such as those who have undergone bone marrow transplantation, neutropenic precautions may also require a patient isolator unit and the use of sterile linens, gowns, gloves, and head and shoe coverings. In such cases, all other items taken into the room should be sterilized or disinfected. The patient's diet also may be modified to eliminate raw fruits and vegetables and to allow only cooked foods and possibly only sterile beverages.
Equipment
Gloves • gowns • masks• neutropenic precautions door card.
Gather any additional supplies, such as a thermometer, stethoscope, and blood pressure cuff, so you don't have to leave the isolation room unnecessarily.
Preparation of equipment
Keep supplies in a clean enclosed cart or in an anteroom outside the room.
Implementation
- After placing the patient in a single room, explain isolation precautions to the patient and his family to ease patient anxiety and promote cooperation.
- Place a neutropenic precautions card on the door to caution those entering the room.
- Wash your hands with an antiseptic agent before putting on gloves, after removing gloves, and as indicated during patient care.
- Wear gloves and gown according to standard precautions, unless the patient's condition warrants a sterile gown, gloves, and a mask.
- Avoid transporting the patient out of the room; if he must be moved, make sure he wears a gown and mask. Notify the receiving department or area so that the precautions will be maintained and the patient will be returned to the room promptly.
- Don't allow visits by anyone known to be ill or infected.
Special considerations
- Don't perform invasive procedures, such as urethral catheterization, unless absolutely necessary because these procedures risk serious infection in the patient with impaired resistance.
- Instruct the housekeeping staff to put on gowns, gloves, and masks before entering the room; no ill or infected person should enter. They should follow the same requirements as the staff, depending on the patient's condition and facility policy.P.130
- Make sure the room is cleaned with freshly prepared cleaning solutions. Because the patient doesn't have a contagious disease, materials leaving the room need no special precautions beyond standard precautions.
Documentation
Document the need for neutropenic precautions on the nursing care plan and as otherwise indicated by your facility.
under:
Infection Control
DISEASE REQUIRING CONTACT PRECAUTIONS
Posted by Admin
| Disease | Precautionary period |
| | |
| Infection or colonization with multidrug-resistant bacteria | Until off antibiotics and culture negative |
| | |
| Clostridium difficile enteric infection | Duration of illness |
| | |
| Escherichia coli disease, in diapered or incontinent patient | Duration of illness |
| | |
| Shigellosis, in diapered or incontinent patient | Duration of illness |
| | |
| Hepatitis A, in diapered or incontinent patient | Duration of illness |
| | |
| Rotavirus infection, in diapered or incontinent patient | Duration of illness |
| | |
| Respiratory syncytial virus infection, in infants and young children | Duration of illness |
| | |
| Parainfluenza virus infection, in diapered or incontinent patient | Duration of illness |
| | |
| Enteroviral infection, in diapered or incontinent patient | Duration of illness |
| | |
| Scabies | Until 24 hours after initiation of effective therapy |
| | |
| Diphtheria (cutaneous) | Duration of illness |
| | |
| Herpes simplex virus infection (neonatal or mucocutaneous) | Duration of illness |
| | |
| Impetigo | Until 24 hours after initiation of effective therapy |
| | |
| Major abscesses, cellulitis, or pressure ulcer | Until 24 hours after initiation of effective therapy |
| | |
| Pediculosis (lice) | Until 24 hours after initiation of effective therapy |
| | |
| Rubella, congenital syndrome | Place infant on precautions during any admission until age 1, unless nasopharyngeal and urine culture are negative for virus after age 3 months |
| | |
| Staphylococcal furunculosis in infants and young children | Duration of illness |
| | |
| Acute viral (acute hemorrhagic) conjunctivitis | Duration of illness |
| | |
| Viral hemorrhagic infections (Ebola, Lassa, Marburg) | Duration of illness |
| | |
| Zoster (chickenpox, disseminated zoster, or localized zoster in immunocompromised patient) | Until all lesions are crusted; requires airborne precautions |
| | |
| Smallpox | Duration of illness; requires airborne precautions |
under:
Infection Control
CONTACT PRECAUTIONS
Contact precautions prevent the spread of infectious diseases transmitted by contact with body substances containing the infectious agent or items contaminated with the body substances containing the infectious agent. Contact precautions apply to patients who are infected or colonized (presence of microorganism without clinical signs and symptoms of infection) with epidemiologically important organisms that can be transmitted by direct or indirect contact. (See Diseases requiring contact precautions, page 128.)
P.127
Effective contact precautions require a single room and the use of gloves and gowns by anyone having contact with the patient, the patient's support equipment, or items soiled with body substances containing the infectious agent. Thorough hand washing and proper handling and disposal of articles contaminated by the body substance containing the infectious agent are also essential.
Equipment
Gloves • gowns or aprons • masks, if necessary • isolation door card • plastic bags.
Gather any additional supplies, such as a thermometer, stethoscope, and blood pressure cuff.
Preparation of equipment
Keep all contact precaution supplies outside the patient's room in a cart or anteroom.
Implementation
- Situate the patient in a single room with private toilet facilities and an anteroom if possible. If necessary, two patients with the same infection may share a room. Explain isolation procedures to the patient and his family.
- Place a contact precautions card on the door to notify anyone entering the room.
- Wash your hands before entering and after leaving the patient's room and after removing gloves.P.128
P.129
- Place any laboratory specimens in impervious, labeled containers, and send them to the laboratory at once. Attach requisition slips to the outside of the container.
- Instruct visitors to wear gloves and a gown while visiting the patient and to wash their hands after removing the gown and gloves.
- Place all items that have come in contact with the patient in a single impervious bag, and arrange for their disposal or disinfection and sterilization.
- Limit the patient's movement from the room. If the patient must be moved, cover any draining wounds with clean dressings. Notify the receiving department or area of the patient's isolation precautions so that the precautions will be maintained and the patient can be returned to the room promptly.
Special considerations
- Cleaning and disinfection of equipment between patients is essential.
- Try to dedicate certain reusable equipment (thermometer, stethoscope, blood pressure cuff) for the patient in contact precautions to reduce the risk of transmitting infection to other patients.
- Remember to change gloves during patient care as indicated by the procedure or task. Wash your hands after removing gloves and before putting on new gloves.
Documentation
Record the need for contact precautions on the nursing care plan and as otherwise indicated by your facility. Document initiation and maintenance of the precautions, the patient's tolerance of the procedure, and any patient or family teaching. Also document the date contact precautions were discontinued.
under:
Infection Control
DISEASES REQUIRING DROPLET PRECAUTIONS
Posted by Admin
| Disease | Precautionary period |
| | |
| Invasive Haemophilus influenzae type b disease, including meningitis, pneumonia, and sepsis | Until 24 hours after initiation of effective therapy |
| | |
| Invasive Neisseria meningitidis disease, including meningitis, pneumonia, epiglottis, and sepsis | Until 24 hours after initiation of effective therapy |
| | |
| Diphtheria (pharyngeal) | Until off antibiotics and two cultures taken at least 24 hours apart are negative |
| | |
| Mycoplasma pneumoniae infection | Duration of illness |
| | |
| Pertussis | Until five days after initiation of effective therapy |
| | |
| Pneumonic plague | Until 72 hours after initiation of effective therapy |
| | |
| Streptococcal pharyngitis, pneumonia, or scarlet fever in infants and young children | Until 24 hours after initiation of effective therapy |
| | |
| Adenovirus infection in infants and young children | Duration of illness |
| | |
| Influenza | Duration of illness |
| | |
| Mumps | For 9 days after onset of swelling |
| | |
| Parvovirus B19 | Maintain precautions for duration of hospitalization when chronic disease occurs in an immunocompromised patient. For patients with transient aplastic crisis or red-cell crisis, maintain precautions for 7 days. |
| | |
| Rubella (German measles) | Until 7 days after onset of rash |
under:
Infection Control
DROPLET PRECAUTIONS
Posted by Admin
Droplet precautions prevent the spread of infectious diseases transmitted by contact of nasal or oral secretions (droplets arising from coughing or sneezing) from the infected patient with the mucous membranes of the susceptible host. This category includes some diseases formerly included in respiratory isolation. The droplets of moisture are heavy and generally fall to the ground within 3′ (1 m); the organisms contained in the droplets don't become airborne or suspended in the air. (See Diseases requiring droplet precautions.)
Effective droplet precautions require a single room (not necessarily a negative-pressure room), and the door doesn't need to be closed. Persons having direct contact with, or who will be within 3′ of the patient, should wear a surgical mask covering the nose and mouth.
When handling infants or young children who require droplet precautions, you may also need to wear gloves and a gown to prevent soiling of clothing with nasal and oral secretions.
Equipment
Masks • gowns, if necessary • gloves • plastic bags • droplet precautions door card.
Gather any additional supplies, such as a thermometer, stethoscope, and blood pressure cuff.
Preparation of equipment
Keep all droplet precaution supplies outside the patient's room in a cart or anteroom.
Implementation
- Place the patient in a single room with private toilet facilities and an anteroom if possible. If necessary, two patients with the same infection may share a room. Explain isolation procedures to the patient and his family.
- Put a droplet precautions card on the door to notify anyone entering the room.
- Wash your hands before entering and after leaving the room and during patient care as indicated.
- Pick up your mask by the top strings, adjust it around your nose and mouth, and tie the strings or adjust the ear loops around your ears for a comfortable fit. If the mask has a flexible metal nose strip, adjust it to fit firmly but comfortably.
- Instruct the patient to cover his nose and mouth with a facial tissue while coughing or sneezing.
- Tape an impervious bag to the patient's bedside so that the patient can dispose of facial tissues correctly.
- Make sure all visitors wear masks when in close proximity with the patient (within 3′) and, if necessary, gowns and gloves.
- If the patient must leave the room for essential procedures, make sure he wears a surgical mask over his nose and mouth. Notify the receiving department or area of the patient's isolation precautions so that the precautions will be maintained and the patient can be returned to the room promptly.
Special considerations
- Before removing your mask, remove your gloves (if worn) and wash your hands.
- Untie the strings and dispose of the mask, handling it by the strings only.
Documentation
Record the need for droplet precautions on the nursing care plan and as otherwise indicated by your facility. Document initiation and maintenance of the precautions, the patient's tolerance of the procedure, and any patient or family teaching. Also document the date droplet precautions were discontinued.
under:
Infection Control
DISEASES REQUIRING AIRBORNE PRECAUTIONS
| Disease | Precautionary period |
| | |
| Chickenpox (varicella) | Until lesions are crusted and no new lesions appear |
| Herpes zoster (disseminated) | Duration of illness |
| Herpes zoster (localized in immunocompromised patient) | Duration of illness |
| Measles (rubeola) Smallpox | Duration of illness |
| Tuberculosis (pulmonary or laryngeal, confirmed or suspected) | Depends on clinical response; patient must be on effective therapy, be improving clinically (decreased cough and fever and improved findings on chest radiograph), and have three consecutive negative sputum smears collected on different days, or TB must be ruled out |
under:
Infection Control
AIRBORNE PRECAUTIONS
Airborne precautions, used in addition to standard precautions, prevents the spread of infectious diseases transmitted by airborne pathogens that are breathed, sneezed, or coughed into the environment. (See Diseases requiring airborne precautions.) This precaution category includes the former categories of acid-fast bacillus (AFB) isolation and respiratory isolation.
Effective airborne precautions require a negative-pressure room with the door kept closed to maintain the proper air pressure balance between the isolation room and the adjoining hallway or corridor. An anteroom is preferred. The negative air pressure must be monitored, and the air is either vented directly to the outside of the building or filtered through high-efficiency particulate air (HEPA) filtration before recirculation.
Respiratory protection must be worn by all persons who enter the room. Such protection is provided by a disposable respirator (such as an N95 respirator or HEPA respirator) or a reusable respirator (such as a HEPA respirator or a powered air-purifying respirator [PAPR]). Regardless of the type of respirator used, the health care worker must ensure proper fit to the face each time she wears the respirator. If the patient must leave the room for an essential procedure, he should wear a surgical mask covering his nose and mouth while out of the room.
Equipment
Respirators (either disposable N95 or HEPA respirators or reusable HEPA respirators or PAPRs) • surgical masks • isolation door card • other personal protective equipment as needed for standard precautions.
Gather any additional supplies, such as a thermometer, stethoscope, and blood pressure cuff.
Preparation of equipment
Keep all airborne precaution supplies outside the patient's room in a cart or anteroom.
Implementation
- Situate the patient in a negative-pressure room with the door closed. If possible, the room should have an anteroom. The negative pressure should be monitored. If necessary, two patients with the same infection may share a room. Explain isolation precautions to the patient and his family.
- Keep the patient's door (and the anteroom door) closed at all times to maintain the negative pressure and contain the airborne pathogens. Put the airborne precautions sign on the door to notify anyone entering the room.
- Pick up your respirator and put it on according to the manufacturer's directions. Adjust the straps for a firm but comfortable fit. Check the respiratory seal. (See Respirator seal check.)
- Instruct the patient to cover his nose and mouth with a facial tissue while coughing or sneezing.
- Tape an impervious bag to the patient's bedside so the patient can dispose of facial tissues correctly.
- Make sure all visitors wear respiratory protection while in the patient's room.
- Limit the patient's movement from the room. If he must leave the room for essential procedures, make sure he wears a surgical mask over his nose and mouth. Notify the receiving department or area of the patient's isolation precautions so that the precautions will be maintained and the patient can be returned to the room promptly.
Special considerations
- Before leaving the room, remove gloves (if worn) and wash your hands. Remove your respirator outside the patient's room after closing the door.P.126
- Depending on the type of respirator and recommendations from the manufacturer, follow your facility's policy and either discard your respirator or store it until the next use. If your respirator is to be stored until the next use, store it in a dry, well-ventilated place (not a plastic bag) to prevent microbial growth. Nondisposable respirators must be cleaned according to the manufacturer's recommendations.
Documentation
Record the need for airborne precautions on the nursing care plan and as otherwise indicated by your facility. Document initiation and maintenance of the precautions, the patient's tolerance of the procedure, and any patient or family teaching. Also document the date airborne precautions were discontinued.
under:
Infection Control
CHOOSING THE RIGHT GLOVE
Posted by Admin
Health care workers may develop allergic reactions as a result of their cumulative exposure to latex gloves and other products containing natural rubber latex. Patients also may have latex sensitivity. (See “Latex allergy protocol†in chapter 8.)
Take the following steps to protect yourself and your patient from allergic reactions to latex:
- Use nonlatex (for example, vinyl or synthetic) gloves for activities that aren't likely to involve contact with infectious materials (such as food preparation and routine cleaning).
- Nonlatex gloves can be worn for activities of short duration, even if contact with infectious materials is possible.
- Use appropriate barrier protection when handling infectious materials. If you choose latex gloves, use powder-free gloves with reduced protein content. Powder in any glove is very drying to skin and may cause problems that may put health care workers at greater risk for exposure to infection if skin is dry and cracked.
- After wearing and removing gloves, wash your hands with soap and dry them thoroughly.
- When wearing latex gloves, don't use oil-based hand creams or lotions (which can cause gloves to deteriorate) unless they've been shown to maintain glove barrier protection.
- Refer to the material safety data sheet for the appropriate glove to wear when handling chemicals.
- Learn procedures for preventing latex allergy, and learn how to recognize the following symptoms of latex allergy: skin rashes, hives, flushing, itching, asthma, shock, and nasal, eye, or sinus symptoms.
- If you have (or suspect you have) a latex sensitivity, use nonlatex gloves, avoid contact with latex gloves and other latex-containing products, and consult a physician experienced in treating latex allergy. Report problems to your supervisor and follow your facility's policy for evaluation.
For known latex allergy
- If you're allergic to latex, consider the following precautions:
- Avoid contact with latex gloves and other products that contain latex.
- Avoid areas where you might inhale the powder from latex gloves worn by other workers.
- Inform your employers and your health care providers (physicians, nurses, dentists, and others).
- Wear a medical identification bracelet.
- Follow your physician's instructions for dealing with allergic reactions to latex.
- Check packages, trays, and kits for items containing latex. Products containing natural rubber latex must be labeled clearly on exterior.
under:
Infection Control
STANDARD PRECAUTIONS - Infection Control
Posted by Admin
Standard precautions were developed by the Centers for Disease Control and Prevention (CDC) to provide the widest possible protection against the transmission of infection. CDC officials recommend that health care workers handle all blood, body fluids (including secretions, excretions, and drainage), tissues, and contact with mucous membranes and broken skin as if they contain infectious agents, regardless of the patient's diagnosis.
Standard precautions encompass much of the isolation precautions previously recommended by the CDC for patients with known or suspected blood-borne pathogens as well as the precautions previously known as body substance isolation. They are to be used in conjunction with other transmission-based precautions: airborne, droplet, and contact precautions.
Standard precautions recommend wearing gloves for any known or anticipated contact with blood, body fluids, tissue, mucous membrane, and nonintact skin. (See Choosing the right glove.) If the task or procedure being performed may result in splashing or splattering of blood or body fluids to the face, a mask and goggles or face shield should be worn. If the task or procedure being performed may result in splashing or splattering of blood or body fluids to the body, a fluid-resistant gown or apron should be worn. Additional protective clothing, such as shoe covers, may be appropriate to protect the caregiver's feet in situations that may expose him to large amounts of blood or body fluids (or both), such as care of a trauma patient in the operating room or emergency department.
Airborne precautions are initiated in situations of suspected or known infections spread by the airborne route. The causative organisms are coughed, talked, or sneezed into the air by the infected person in droplets of moisture. The moisture evaporates, leaving the microorganisms suspended in the air to be breathed in by susceptible persons who enter the shared air space. Airborne precautions recommend placing the infected patient in a negative-pressure isolation room and the wearing of respiratory protection by all persons entering the patient's room.
Droplet precautions are used to protect health care workers and visitors from mucous membrane contact with oral and nasal secretions of the infected individual.
Contact precautions use barrier precautions to interrupt the transmission of specific epidemiologically important organisms by direct or indirect contact. Each institution must establish an infection control policy that lists specific barrier precautions.
Equipment
Gloves • masks • goggles, glasses with side pieces, or face shields • gowns or aprons • resuscitation masks • bags for specimens • Environmental Protection Agency (EPA)–registered tuberculocidal disinfectant or diluted bleach solution (diluted between 1:10 and 1:100, mixed fresh daily), or both, or EPA-registered disinfectant labeled effective against hepatitis B virus (HBV), hepatitis C virus (HCV), mycobacteria (including tuberculosis), and human immunodeficiency virus (HIV), provided that the surface hasn't been contaminated
with agents or volumes of or concentrations of agents for which higher level disinfection is recommended.
P.123
with agents or volumes of or concentrations of agents for which higher level disinfection is recommended.
Implementation
- Wash your hands immediately if they become contaminated with blood or body fluids, excretions, secretions, or drainage; also wash your hands before and after patient care and after removing gloves. Hand washing removes microorganisms from your skin. If your hands aren't visibly soiled, or it isn't possible to wash your hands, an alcohol-based hand rub can be used for routine decontamination.
- Wear gloves if you will or could come in contact with blood, specimens, tissue, body fluids, secretions or excretions, mucous membrane, broken skin, or contaminated surfaces or objects.
- Change your gloves and wash your hands or use a hand sanitizer between patient contacts to avoid cross-contamination.
- Wear a fluid-resistant gown, face shield, or goggles and a mask during procedures likely to generate splashing or splattering of blood or body fluids, such as surgery, endoscopic procedures, dialysis, assisting with intubation or manipulation of arterial lines, or any other procedure with potential for splashing or splattering of body fluids.
- Handle used needles and other sharp instruments carefully. Don't bend, break, reinsert them into their original sheaths, remove needles from syringes, or unnecessarily handle them. Discard them intact immediately after use into a puncture-resistant disposal box. Use tools to pick up broken glass or other sharp objects. Use safety devices accordingP.124
to the instructions provided by the manufacturer. Activate all safety mechanisms on sharp devices immediately after use, even if the sharps disposal container is very close. Evaluate your work practices to make sure you're working safely, both for your own protection and for the protection of your patients and coworkers. These measures reduce the risk of accidental injury or infection. When available, use a needleless I.V. system. - Immediately notify your employee health provider of all needle-stick or other sharp object injuries, mucosal splashes, or contamination of open wounds or nonintact skin with blood or body fluids to allow investigation of the incident and appropriate care and documentation.
- Properly label all specimens collected from patients, and place them in plastic bags at the collection site. Attach requisition slips to the outside of the bag.
- Place all items that have come in direct contact with the patient's secretions, excretions, blood, drainage, or body fluids—such as nondisposable utensils or instruments—in a single impervious bag or container before removal from the room. Place linens and trash in single bags of sufficient thickness to contain the contents.
- While wearing the appropriate personal protective equipment, promptly clean all blood and body fluid spills with detergent and water followed by an EPA-registered tuberculocidal disinfectant or diluted bleach solution (diluted between 1:10 and 1:100, mixed daily), or both, or an EPA-registered disinfectant labeled effective against HBV and HIV, provided that the surface hasn't been contaminated with agents or volumes of or concentrations of agents for which higher-level disinfection is recommended.
- Disposable food trays and dishes aren't necessary.
- If you have an exudative lesion, avoid all direct patient contact until the condition has resolved and you've been cleared by the employee health provider.
- If you have dermatitis or other conditions resulting in broken skin on your hands, avoid situations where you may have contact with blood and body fluids (even though gloves could be worn) until the condition has resolved and you've been cleared by the employee health provider.
Special considerations
- Standard precautions, such as hand hygiene and appropriate use of personal protective equipment, should be routine infection control practices.
- Keep mouthpieces, resuscitation bags, and other ventilation devices nearby to eliminate the need for emergency mouth-to-mouth resuscitation, thus reducing the risk of exposure to body fluids.
- NURSING ALERT Because you may not always know what organisms may be present in every clinical situation, you must use standard precautions for every contact with blood, body fluids, secretions, excretions, drainage, mucous membranes, and nonintact skin. Use your judgment in individual cases about whether to implement additional isolation precautions, such as airborne, droplet, or contact precautions or a combination of them. What's more, if your work requires you to be exposed to blood, you should receive the HBV vaccine series.
Complications
Failure to follow standard precautions may lead to exposure to blood-borne diseases or other infections and to all the complications they may cause.
Documentation
Record any special needs for isolation precautions on the nursing care plan and as otherwise indicated by your facility. Document patient and family teaching about isolation precautions.
under:
Infection Control
REPORTABLE DISEASES CHECKLIST
Because reporting laws vary from state to state, this list isn't conclusive and may be changed periodically. Local agencies report certain diseases to their state health departments, which in turn determine which diseases are reported to the Centers for Disease Control and Prevention (CDC).
Acquired immunodeficiency syndrome (AIDS)
Anthrax
Botulism, foodborne
Botulism, infant
Botulism, other (wound and unspecified)
Brucellosis
Chancroid
Chlamydia trachomatis, genital infections
Cholera
Coccidioidomycosis
Cryptosporidiosis
Cyclosporiasis
Diphtheria
Ehrlichiosis
Encephalitis/meningitis, arboviral
Enterohemorrhagic Escherichia coli
Giardiasis
Gonorrhea
Haemophilus influenza, invasive disease
Hansen's disease
Hantavirus pulmonary syndrome
Hemolytic uremic syndrome, postdiarrheal
Hepatitis A, acute, chronic
Hepatitis B, acute, chronic
Hepatitis B, perinatal infection
Hepatitis C, acute, chronic
Human immunodeficiency virus (HIV) infection
Legionellosis
Listeriosis
Lyme disease
Malaria
Measles
Meningococcal infections
Mumps
Pertussis
Plague
Poliomyelitis, paralytic
Psittacosis
Q fever
Rabies, animal
Rabies, human
Rheumatic fever
Rocky Mountain spotted fever
Rubella
Salmonellosis
Shigellosis
Streptococcal disease, invasive, Group A
Streptococcal toxic-shock syndrome
Streptococcus pneumonia, drug resistant, invasive disease
Streptococcus pneumonia, invasive in children over age 5
Syphilis, all stages
Syphilis, primary and secondary
Syphilis, congenital
Tetanus
Toxic shock syndrome
Trichinosis
Tuberculosis
Tularemia
Typhoid fever
Varicella
Yellow fever
under:
Infection Control
REPORTABLE DISEASES
Posted by Admin
Certain contagious diseases must be reported to local and state public health officials and, ultimately, to the Centers for Disease Control and Prevention (CDC). (See Reportable diseases checklist.) Typically, these diseases fit one of two categories:
P.122
those reported individually based on a definitive or suspected diagnosis and those reported by the number of cases per week. The most commonly reported diseases include hepatitis, measles, salmonellosis, shigellosis, syphilis, and gonorrhea.
- NURSING ALERT Although smallpox isn't listed on the CDC reportable diseases checklist, it's reportable. Selected microorganisms are suspected as potential agents of biological warfare and are reportable immediately to the local or state health department. These agents include anthrax, botulinum toxin, plague, smallpox, and tularemia.
In most states, the patient's physician must report communicable diseases to health officials. In hospitals, the infection control practitioner or epidemiologist reports them. The laboratory must also report organisms associated with reportable diseases. However, you should know the reporting requirements and procedures. Fast, accurate reporting helps identify and control infection sources, prevent epidemics, and guide public health planning and policy.
Equipment
Nursing procedure or infection control manual • disease-reporting form, if available.
Implementation
- Make sure reportable diseases are listed and that the list is available to all shifts.
- Know your facility's protocol for reporting diseases. Typically, you'll contact the infection control practitioner or epidemiologist. If this person isn't available, contact your supervisor or the infectious disease physician on call.
Documentation
Document any diseases reported to the infection control practitioner, the practitioner's name, and the date and time of the report.
under:
Infection Control
REMOVING CONTAMINATED GLOVES
Posted by Admin
Proper removal techniques are essential for preventing the spread of pathogens from gloves to your skin surface.
Follow these steps carefully.
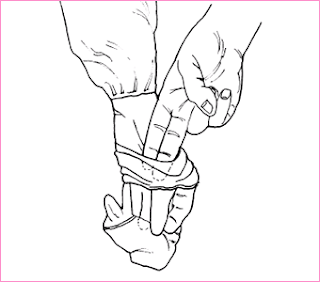
1. Using your left hand, pinch the right glove near the top. Avoid allowing the glove's outer surface to buckle inward against your wrist.

2. Pull downward, allowing the glove to turn inside out as it comes off. Keep the right glove in your left hand after removing it.

3. Now insert the first two fingers of your ungloved right hand under the edge of the left glove. Avoid touching the glove's outer surface or folding it against your left wrist.

4. Pull downward so that the glove turns inside out as it comes off. Continue pulling until the left glove completely encloses the right one and its uncontaminated inner surface is facing out.
under:
Infection Control
Face Mask - Standard

under:
Infection Control
USE OF ISOLATION EQUIPMENT
Posted by Admin
Isolation procedures may be implemented to prevent the spread of infection from patient to patient, from the patient to health care workers, or from health care workers to the patient. They may also be used to reduce the risk of infection in immunocompromised patients. Central to the success of these procedures is the selection of the proper equipment and the adequate training of those who use it.
Equipment
Materials required for isolation typically include barrier clothing, an isolation cart or anteroom for storing equipment, and a door card announcing that isolation precautions are in effect.
Barrier clothing:
Gowns • gloves • goggles • masks. Each staff member must be trained in their proper use.
Isolation supplies:
Labels • tape • laundry bags (and water-soluble laundry bags, if used) • plastic trash bags.
An isolation cart may be used when the patient's room has no anteroom. It should include a work area (such as a pull-out shelf), drawers or a cabinet area for holding isolation supplies and, possibly, a pole on which to hang coats or jackets.
Preparation of equipment
Remove the cover from the isolation cart if necessary, and set up the work area. Check the cart or anteroom to ensure that correct and sufficient supplies are in place for the designated isolation category.
Implementation
- Remove your watch (or push it well up your arm) and your rings according to facility policy. These actions help to prevent the spread of microorganisms hidden under your watch or rings.
- Wash your hands before putting on gloves to prevent the growth of microorganisms under gloves.
Putting on isolation garb
- Put the gown on and wrap it around the back of your uniform. Tie the strings or fasten the snaps or pressure-sensitive tabs at the neck. Make sure your uniform is completely covered to prevent contact with the patient or his environment.
- Place the mask snugly over your nose and mouth. Secure ear loops around your ears or tie the strings behind your head high enough so the mask won't slip off. If the mask has a metal strip, squeeze it to fit your nose firmly but comfortably. (See Putting on a face mask.) If you wear eyeglasses, tuck the mask under their lower edge. If goggles are worn, put them on at this time.
- Put on the gloves. Pull the gloves over the cuffs to cover the edges of the gown's sleeves.
Removing isolation garb
- Remember that the outside surfaces of your barrier clothes are contaminated.
- While wearing gloves, untie the gown's waist strings.
- With your gloved left hand, remove the right glove by pulling on the cuff, turning the glove inside out as you pull.P.120
P.121
Don't touch any skin with the outside of either glove. (See Removing contaminated gloves.) Then remove the left glove by wedging one or two fingers of your right hand inside the glove and pulling it off, turning it inside out as you remove it. Discard the gloves in the trash container. - Untie the neck straps of your gown. Grasp the outside of the gown at the back of the shoulders and pull the gown down over your arms, turning it inside out as you remove it to ensure containment of the pathogens.
- Holding the gown well away from your uniform, fold it inside out. Discard it in the laundry or trash container as necessary.
- If the sink is inside the patient's room, wash your hands and forearms with soap or antiseptic before leaving the room. Turn off the faucet using a paper towel and discard the towel in the room. Grasp the door handle with a clean paper towel to open it, and discard the towel in a trash container inside the room. Close the door from the outside with your bare hand.
- Remove the mask last to prevent contaminating your face or hair in the process. Untie your mask, holding it only by the strings. Discard the mask in the trash container. Remove goggles.
- If the sink is in an anteroom, wash your hands and forearms with soap or antiseptic after leaving the room.
Special considerations
- If airborne precautions are required, a particulate respirator should be worn rather than a surgical mask.
- Use gowns, gloves, goggles, and masks only once, and discard them in the appropriate container before leaving a contaminated area. If your mask is reusable, retain it for further use unless it's damaged or damp. Be aware that isolation garb loses its effectiveness when wet because moisture permits organisms to seep through the material. Change masks and gowns as soon as moisture is noticeable or according to the manufacturer's recommendations or your facility's policy.
- At the end of your shift, restock used items for the next person. After patient transfer or discharge, return the isolation cart to the appropriate area for cleaning and restocking of supplies. An isolation room or other room prepared for isolation purposes must be thoroughly cleaned and disinfected before use by another patient.
under:
Infection Control
PROPER HANDWASHING TECHNIQUE
Posted by Admin
To minimize the spread of infection, follow these basic handwashing instructions. With your hands angled downward under the faucet, adjust the water temperature until it's comfortably warm.
Add soap and work up a generous lather by scrubbing vigorously for 10 seconds. Be sure to clean beneath fingernails, around knuckles, and along the sides of fingers and hands.
Rinse your hands completely to wash away suds and microorganisms. Pat dry with a paper towel. To prevent recontaminating your hands on the faucet handles, cover each one with a dry paper towel when turning off the water.
under:
Infection Control
Search
Archives
-
▼
2010
(55)
-
▼
May
(16)
- CONDITIONS AND TREATMENTS REQUIRING NEUTROPENIC PR...
- NEUTROPENIC PRECAUTIONS
- DISEASE REQUIRING CONTACT PRECAUTIONS
- CONTACT PRECAUTIONS
- DISEASES REQUIRING DROPLET PRECAUTIONS
- DROPLET PRECAUTIONS
- DISEASES REQUIRING AIRBORNE PRECAUTIONS
- AIRBORNE PRECAUTIONS
- CHOOSING THE RIGHT GLOVE
- STANDARD PRECAUTIONS - Infection Control
- REPORTABLE DISEASES CHECKLIST
- REPORTABLE DISEASES
- REMOVING CONTAMINATED GLOVES
- Face Mask - Standard
- USE OF ISOLATION EQUIPMENT
- PROPER HANDWASHING TECHNIQUE
-
▼
May
(16)
Links
-
a duck can't walk wi...8 years ago
-